By: Ash Chandrakapure, Social Chair, The Associate Board IntroductionFor individuals experiencing homelessness in Chicago, recovering from illness or injury can seem like an insurmountable challenge. Many are discharged from hospitals without the proper support to heal, often facing a difficult choice between returning to the streets or to shelters where recovery is nearly impossible. Medical respite care is a game-changer, providing not only temporary housing but also the healthcare services necessary for individuals to transition from hospitalization to full recovery. | |||||
| |||||
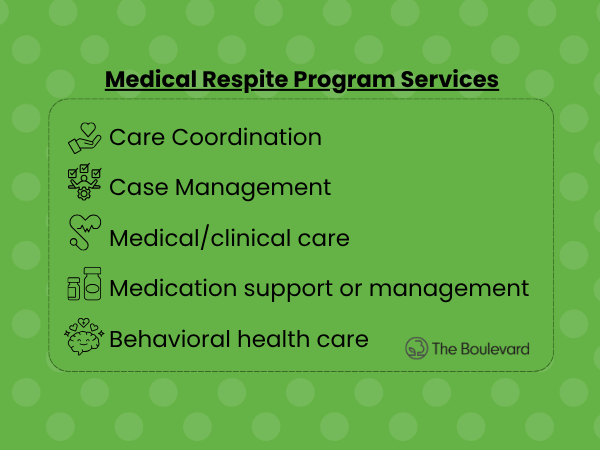
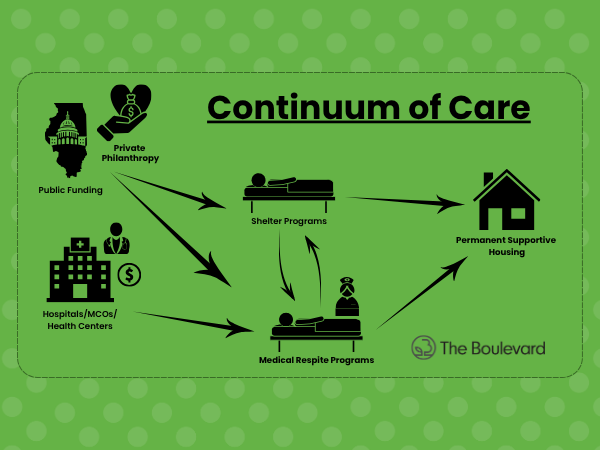
How Medical Respite Care Differs from Other ServicesIn many ways, medical respite care bridges the gap between hospitals and shelters. Shelters may offer a place to sleep, and hospitals focus on treating acute conditions, but medical respite care takes a more integrated approach. It combines the necessary medical services with stable housing, which is crucial for individuals who are not yet able to care for themselves after being discharged. As the U.S. Department of Health and Human Services (HHS) highlights, this combination of medical care and housing is vital for reducing complications and supporting a sustainable recovery.(2) By providing both medical care and stability, these programs ensure that individuals can heal properly, minimizing the risks of complications that could lead to further hospitalizations. | |||||
| |||||
Challenges and Opportunities for GrowthDespite its proven success, many medical respite care programs face challenges, particularly when it comes to funding and capacity. As homelessness continues to rise, so does the need for more respite care beds, but limited resources make it difficult for many programs to expand.
Adding to these concerns, potential cuts to federal funding pose a serious threat to medical respite care programs nationwide.(6) Recent shifts in government budgets have put social services at risk, making it harder for programs like The Boulevard of Chicago to secure the financial support they need. Reductions in Medicaid reimbursements, housing assistance programs, and public health funding will significantly impact the ability of respite care facilities to provide essential services. Without adequate financial backing, these programs will struggle to maintain staffing, expand capacity, or even continue operations—leaving many homeless individuals without a safe place to recover. However, these challenges also present opportunities for growth. As awareness of the effectiveness of medical respite care grows, there is a chance to strengthen partnerships between hospitals, local governments, and nonprofit organizations. Such collaborations could bolster funding, expand capacity, and improve accessibility for those who need it most. Advocating for continued and increased funding at both state and federal levels is crucial to ensuring these life-saving programs remain available. | |||||
|
If this cause resonates with you, consider supporting programs like The Boulevard of Chicago—whether through advocacy, donations, or volunteering—to help ensure that more individuals have access to the care and support they deserve. |
Sources:
National Health Care for the Homeless Council. (n.d.). Models of medical respite care. National Health Care for the Homeless Council. Retrieved March 8, 2025, from
https://nhchc.org/resource/models-of-medical-respite-care/U.S. Department of Health and Human Services (HHS). (2020). Medical respite care: A critical intervention for homeless populations. HHS Resources. Retrieved March 8, 2025, from https://www.hhs.gov/ash/oah/resources-and-training/homeless-populations/index.html
Bergen-Cico, D., Graw, S., & Vargo, A. (2017). Medical respite care and its impact on hospital readmissions and emergency room visits for homeless populations. American Journal of Public Health, 107(11), 1803-1810. https://doi.org/10.2105/AJPH.2017.303985
Healthcare for the Homeless Clinicians Network (HHCN). (2019). The role of medical respite care in improving health outcomes for homeless individuals. HHCN Policy Brief. Retrieved March 8, 2025, from https://www.nhchc.org/wp-content/uploads/2019/06/Respite-Policy-Brief.pdf
National Alliance to End Homelessness (NAEH). (2022). The state of homelessness in America: Trends and challenges in providing healthcare. NAEH Report. Retrieved March 8, 2025, from https://endhomelessness.org/resource/state-of-homelessness-2022/
National Health Care for the Homeless Council. (2025, March 8). The countdown is on: Congress is deciding how and where to cut Medicaid. National Health Care for the Homeless Council. Retrieved March 8, 2025, from https://nhchc.org/the-countdown-is-on-congress-is-deciding-how-and-where-to-cut-medicaid/?utm_source=chatgpt.com